While the US administration obsesses with pointing DOGE at relatively small levels of governmental expenditure in areas such as USAID and the Department of Education, when it comes to US healthcare, there are levels of cost inefficiencies and improved outcomes that could reach trillions of dollars if managed effectively.
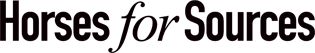
In fact, if US healthcare were its own country, its annual spending of $5.2 trillion would make it the world’s third-largest country by GDP. Yet, the US has amongst the worst health outcomes among OECD countries, with the lowest life expectancies for both men and women, and has not been able to address obesity and mental health epidemics:
At the same time, the prevalence of chronic conditions rises without checks. So, in some ways, DOGE hacking away at what it considers wasteful spending of taxpayer’s money is welcome. In that context, we provide DOGE recommendations on where such cuts should be in healthcare.
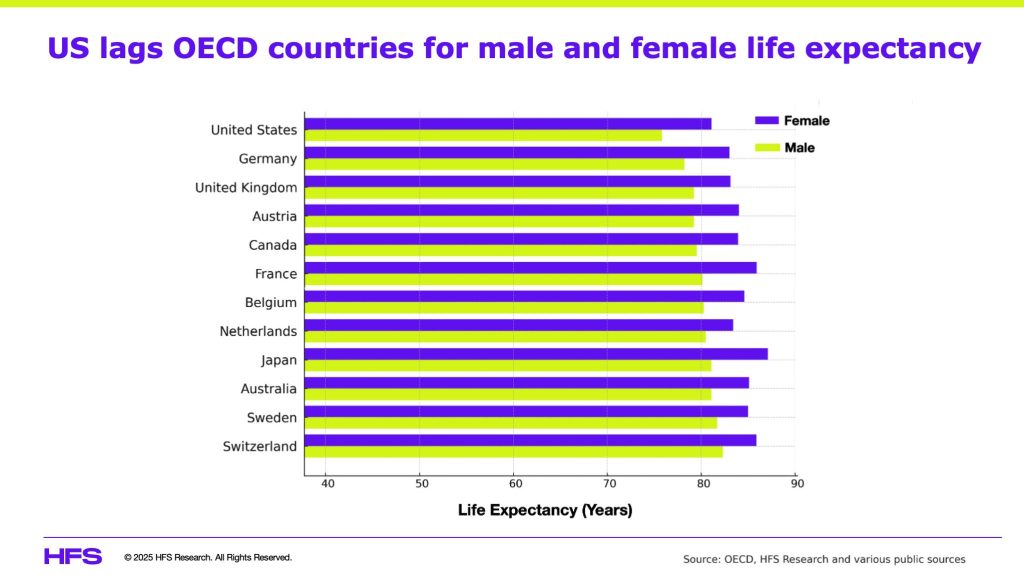
These three main categories drive the cost of healthcare in the US:
- Compensation for everyone in the healthcare ecosystem (doctors, nurses, administrators),
- Therapies (R&D, medication, devices),
- Administration (regulations, processes, payments).
While compensation and therapies have opportunities to be streamlined and reduced, the administration cost can be hacked with DOGE recklessness without legislative action and yield better outcomes:
US healthcare admin costs double that of comparable countries with worse health outcomes
According to an analysis by the Mercatus Center, the US had upwards of 42,000 regulations instituted by the Department of Health and Human Services as of 2020. These regulations are additive to state and local regulations. No wonder the US spends about 7% of its per-capita healthcare spending of ~$15,000 (2024) on administrative processes, twice that of comparable countries (Austria, UK, France, Germany).
While regulations are essential to ensure rules are applied evenly, health consumers are protected, proper care is rendered, and payers, providers, pharma’s, and other ancillary organizations deliver their services as health fiduciary agents. However, when those regulations add costs materially and inhibit or delay care, it is time to eliminate them.
There is a laundry list of regulations that have done nothing but add costs and risk to human life. Some that require immediate attention are:
- Prior authorizations (PA): This process requires providers or consumers to seek approval from health insurers before getting treatment. PAs lead to delayed treatments and often abandoned treatment, causing health risks to patients. They also require providers to add staff to manage PAs. Analysis of 2021 Medicare data shows that 95% of all PAs were approved. This reflects the enormous cost and health risk burden being unnecessarily imposed on the US healthcare system.
- HIPAA: While the 1996 law’s intention is still valid, its overuse has added cost and made data sharing unnecessarily complicated. Given that pre-existing conditions cannot be factored into underwriting risk, it is time to readjust how HIPAA is utilized…privacy is different in the 21st century than in the last one.
- Interoperability: CMS rules to drive interoperability are based on a fundamentally wrong premise. Healthcare data belongs to consumers, not the government or health insurance companies. Consumers alone must decide who, when, what purpose, and for how long their health data can be used. CMS or other healthcare entities have no business in determining these rules. Elimination of interoperability rules should release significant resources and administrative burdens. Instead, private-public efforts must create a consumer-facing healthcare data aggregation solution…my data on my mobile app.
Recommendation to DOGE: Eliminate any regulation that does not explicitly reduce cost and improve health outcomes within 12 months.
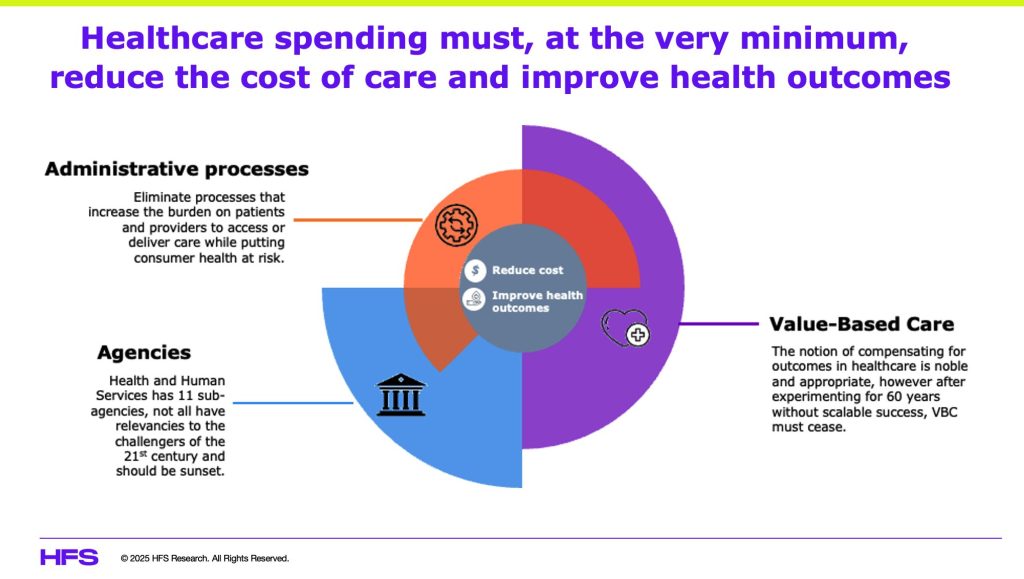
There is nothing valuable about value-based care
Since the 1960s, the US has been experimenting with value-based care (VBC) with little to show. CMS defines this concept as designing care to focus on quality, provider performance, and the patient experience. Over the last 60 years, CMS has driven countless programs (see Exhibit 3), yet estimates suggest that less than 25% of all Medicare contracts are aligned to some form of VBC. VBC is a dead concept, given that it seeks to impose an insurance construct on care delivery, which has no proof of working consistently and at scale over time.
While the idea of holding everyone in the healthcare ecosystem accountable for costs and outcomes is important, there is no precedent for it in any part of the world…yet. There may be private-public options to achieve a capitated model based on social determinants of health; however, those are in the realm of possibilities rather than current realities.
Recommendation to DOGE: Sunset all CMS VBC programs immediately.
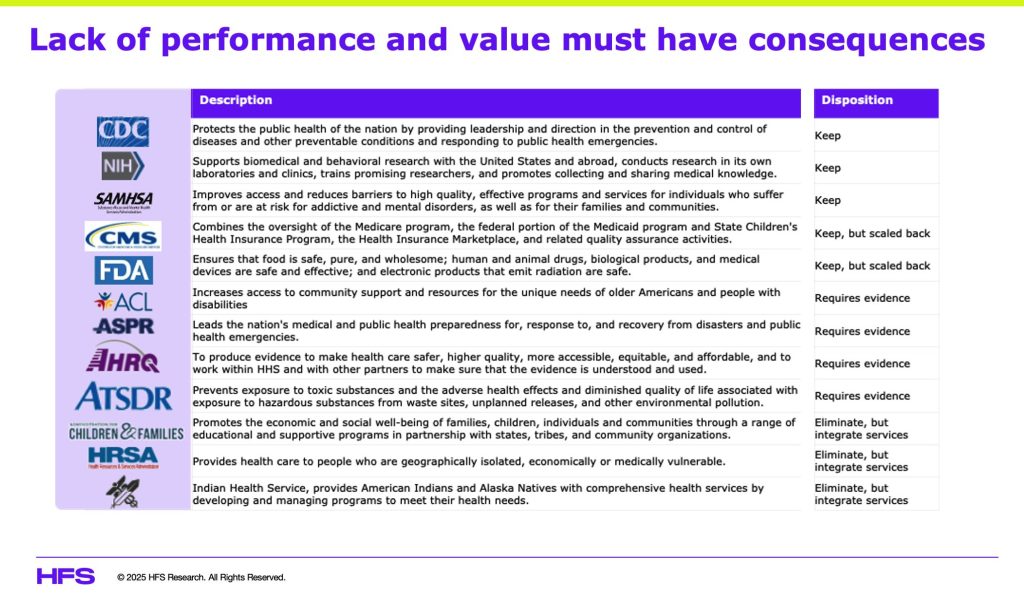
DHHS needs organizational simplicity and 21st-century purpose
According to the US Department of Treasury, in fiscal 2025, the Department of Health and Human Services (DHHS) will account for 26% of all US government spending. It is the largest agency by budget and influences the largest category of spend. Yet, the US health outcomes continue to decline and are a laggard amongst OECD nations seen through the lens of life expectancy, prevalence of chronic conditions, and epidemics (opioid, obesity, mental health). This is an unacceptable story requiring an organizational overhaul (see Exhibit 3) to reduce costs by simplifying and eliminating what does not work.
DHHS has 11 sub-agencies, three focused on human services and eight on health. The purpose of many of these sub-agencies either overlap or are not relevant anymore. Changing demographics, challenges of the 21st century, and advanced technologies justify rationalizing these agencies. There are three categories for the disposition of DHHS agencies:
- Keep: These are agencies whose purpose is central to critical programs that prevent pandemics or epidemics while allowing the US to keep leading on disease management, such as CDC, NIH, and SAMHSA. Other agencies should be allowed to function but scaled back through the elimination of wasteful administrative functions. Agencies like CMS and FDA can leverage technologies and streamlined processes to address their mandates.
- Requires evidence: These are agencies whose purpose needs validation through outcomes they delivered or influenced over the last five years. Agencies like ACL, ASPR, AHRQ, and ATSDR may have fulfilled their mission, but they may need to be sunset.
- Eliminate: These are agencies whose purpose does not support a stand-alone focus but can be folded into other agencies for services. Indian Health Services or Health Resources and Services Administration (HRSA) must be folded into CMS, given that the beneficiaries could use Medicare or Medicaid.
Recommendation to DOGE: Eliminate agencies that can not quantify their impact on lowering healthcare costs or improving health outcomes.
The Bottom Line: Addressing the low-hanging fruit of US healthcare can yield immediate cost relief while improving health outcomes
It is unconscionable that the US spends ~20% of our GDP, the highest both in aggregate and as a percentage of GDP, yet delivers amongst the worst health outcomes (life expectancy, infant mortality, prevalence of chronic conditions, substance abuse). To blame is the healthcare ecosystem’s complexity (administration, cost of care, clinical expertise) in terms of costs and outcomes. It is due for another transformation but must be a private-public partnership. While that level of collaboration may take some doing, the low-hanging fruits of reducing admin processes, eliminating the delusions of VBC, and rationalizing DHHS can bring some relief.
Posted in : Analytics and Big Data, Healthcare, Politics