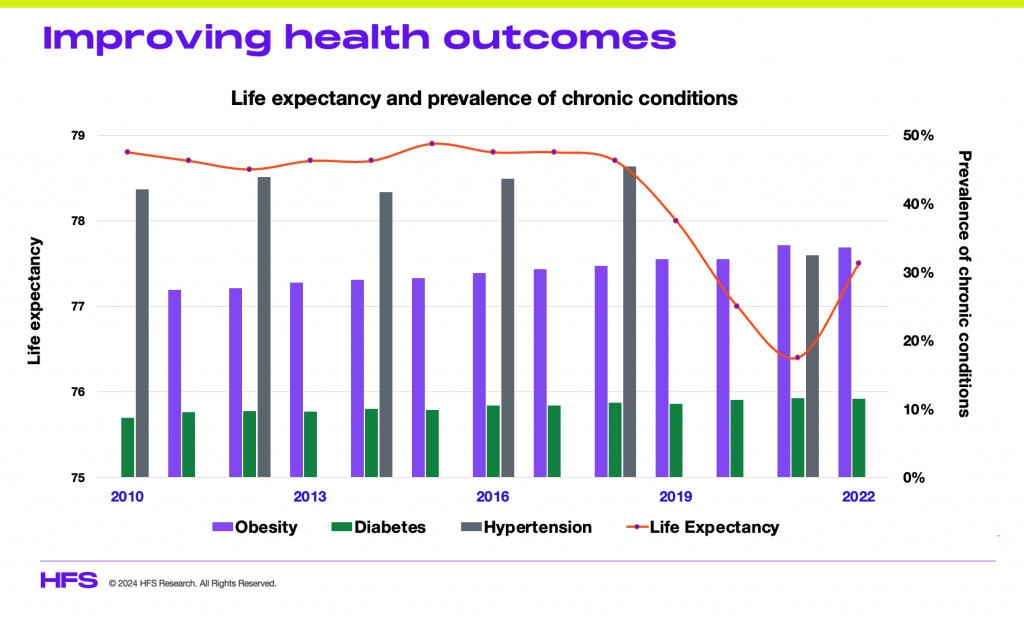
Being a Brit transplanted in the US, it is bizarre to me that the state of healthcare is not an election issue. In the UK, it’s the constant political hot potato – never enough funding, never enough nurses, doctors on strike, massive waiting lists for patients, etc. However, from my own personal experience, the waitlists are just as frustrating in the States, the IT systems are woefully integrated (and some actually worse than the UK’s NHS), the patient experience is very “transactional,” reactive, and rarely joined up, despite $5 trillion annually propping up this mammoth house of cards.
Fortunately, at HFS, we have a deep focus on healthcare and life sciences, which has taught me personally a lot about the core issues, so I asked our fearless healthcare lead analyst, Rohan Kulkarni, to name six big things we can address to fix these problems while American voters obsess about anything but their healthcare…
All attributes of the quadruple aim of care continue to head in the wrong direction
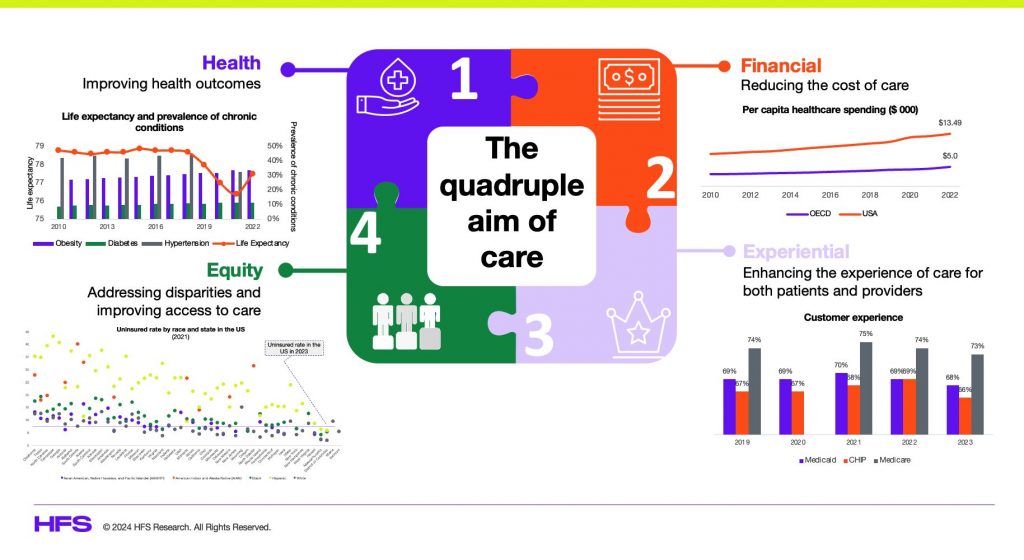
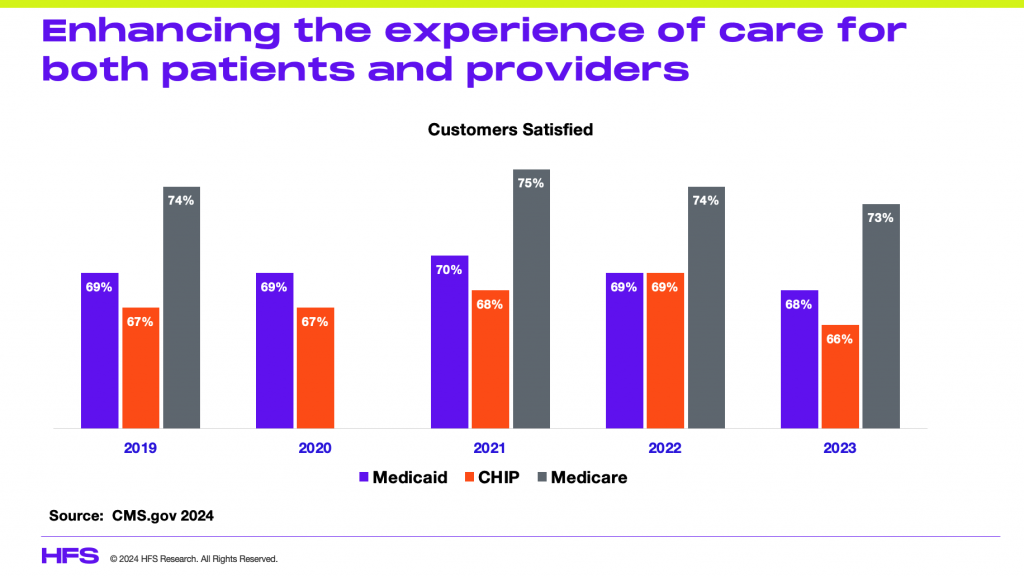
Given the strong financial incentives to perpetuate a system that operates without responsibility or accountability, nothing can be done to fix this sick care paradigm. At HFS Research, we measure the performance of US healthcare across the quadruple aim of care (see Exhibit below) – to reduce the cost of care, enhance the experience of care, improve health outcomes, and address health equities. Despite strong evidence of all elements of the quadruple aim of care failing its health consumers, there are no meaningful catalysts to trigger a change in direction:
However, there are 6 things that are still possible that may give us some relief…
1. Eat healthy and get off the couch
There is significant clinical evidence to suggest that those who are mindful of what they eat and maintain an active lifestyle tend to remain healthy compared to those who don’t. DNA certainly plays a part, but it is likely that a diet of saturated fats and high cholesterol combined with a sedentary lifestyle is not consistent with disease-free, high quality of life, and long life spans. It is, therefore, incumbent upon each of us to practice a healthy lifestyle (nutrition, activity, hygiene) if we want to remain relatively disease-free and postpone those healthcare visits.
2. Employers fire your health insurers
Despite all the fuss about AI, employees will likely remain an employer’s ultimate asset for the foreseeable future. It is, therefore, an economic imperative for employers to keep their employees healthy (sick employee = cost, healthy employee = revenues). To support a healthy employee population, employers must really explore underwriting the medical risk of their employees, especially those that are profitable, in a services business, and have limited liabilities. Those who are already self-insured must consider creating direct-to-provider constructs with a reasonable capitated fee that eliminates all those foolish administrative burdens like prior authorization and claims processing while getting a better quality of care at a lower price.
3. Consumers embrace subscription-based primary care
President Obama said in the throes of the Affordable Care Act fights of 2013 that healthcare would be cheaper than your monthly cell phone bill. He was not kidding. Subscription for digital health-enabled primary care is as low as $9.00 per month if you are an Amazon Prime member of OneMedical. Other providers charge between $50 and $200. Some even include a formulary with up to 200 most commonly prescribed medications. This is a catalyst for us to re-embrace primary care without the hassles of prior authorization and coverage constraints to manage our health proactively.
4. Forget CVS and Walgreens for Rx
Alternatives like Mark Cuban Cost Plus and Amazon pharmacy are making prescriptions significantly less expensive and easier to access, especially if they are generics. Each of these has a different approach, yet they are significantly less expensive than chain pharmacies, deliver to our homes, provide transparent pricing, and are becoming the go-to for generics. Employers and consumers must begin to include such alternatives in their prescription filling process to reduce their healthcare costs and stress.
5. Medical IoT and wearables will save us from us
The sick care paradigm that envelopes us is one driven by a demand-based intervention construct. It is where we, the individuals, decide how we feel and when to seek help. Given the proliferation of medical IoT, wearables, and the inclusion of AI to support diagnostics, we are at an inflection point to reset the care delivery paradigm. Consider leveraging all these technologies to enable a need-based intervention. Let the devices and data inform the clinicians when and for what to intervene. Employers and consumers can drive this shift as part of their direct-to-provider contracts to allow for continuous monitoring and need-based interventions that arguably save significant costs while improving health outcomes by intervening as needed and accurately.
6. Make healthcare equitable to all US citizens
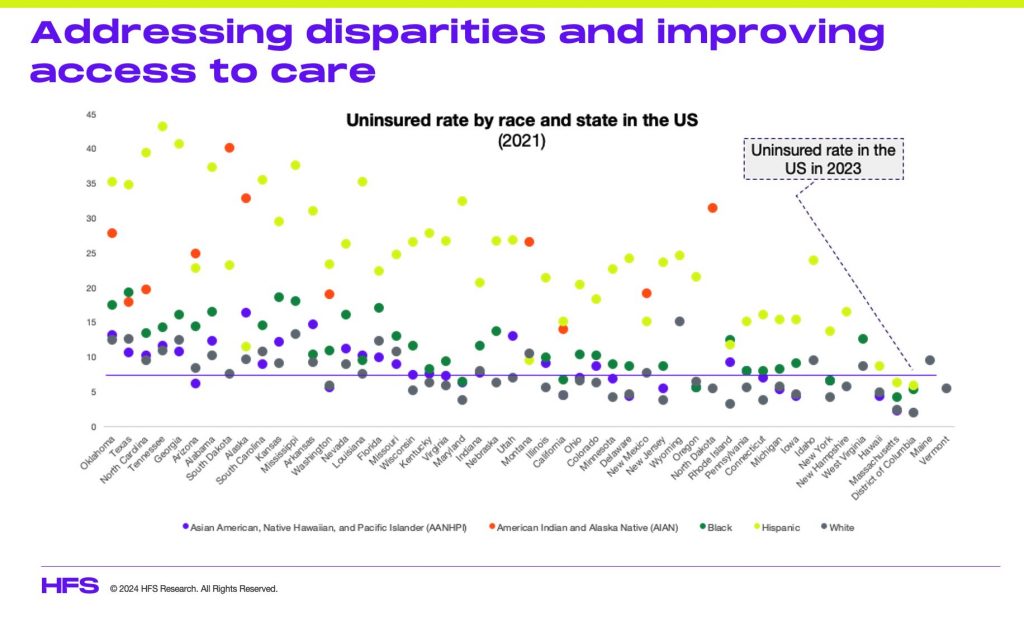
Healthcare protocols are biased towards the majority demographics (white, urban, educated, and wealthy), leaving minorities and the underprivileged underserved and uncared for. Private-public partnerships must address these communities, given they are critical workforce levers if cared for. Consequently, community-based care constructs that incorporate social determinants attract community-specific resources to be the first line of triage that addresses trust gaps and addresses diseases that communities are pre-disposed to, e.g., Pacific Islanders are pre-disposed to obesity, as are African Americans to diabetes. Community and underserved focus is key to democratizing care to help improve local economies, address health equities, and improve health outcomes.
The Bottom Line: We are SOL in this sick care paradigm, but consumers and employers are best positioned to make incremental changes on their own that can be material.
The reality is that we can not keep doing the same things and expect different results. We must change what we do, leverage technologies, and be bold enough to experiment outside the legacy sick care paradigm. Short of that, our choice is to sit on the curb and whine about how our healthcare system sucks!
Posted in : Analytics and Big Data, Artificial Intelligence, Healthcare, Life Sciences